February 2013, v.1.58
Current version: v.2.0
Updated: June 2021
Feedback/Comments :: View Release Notes
- Overview
- Methodology
- Background
- Biochemical Pathway and Nutrition Treatment Rationale
- Nutrition Assessment
- Comparative Standards
- Nutrition Problem Identification
- Nutrition Intervention
- Nutrition Recommendations
- 1. Nutrition interventions during illness, trauma or surgery
- 2. Nutrition management and Branched chain amino acid (BCAA) blood concentrations
- 3. Thiamin supplementation
- 4. Nutrition interventions during pregnancy, at delivery and during the postpartum period
- 5. Nutrition interventions and liver transplantation
- Monitoring and Evaluation
- Resources
- Benefits and Harms of Implementing the Recommendations
- Barriers to Implementation
- Areas for Future Research
- List of Tables
-
Literature Evidence Summary Tables
- T.1 MSUD Phenotypes
- T.2 Laboratory and Clinical Findings for Classical MSUD
- T.3 Nutrient Recommended Intake and Sources in the Dietary Treatment of Well Individuals with MSUD
- T.4 Recommended Dietary PRO, BCAA and Energy Intake
- T.5 Nutrition Problem Identification for MSUD based on the International Dietetics and Nutrition Terminology Reference Manual, 3rd Edition
- T.6 Recommendations for the Nutritional Monitoring of Individuals with MSUD
- T.7 Classification of Medical Foods for MSUD
MSUD Toolkit Tables- T.8 Recommended Nutrient Intake for Newborn Infant with MSUD
- T.9 Medical Food and Breast Milk Composition for Case 3.1
- T.10 Calculation of Formula Mix to Meet Recommended Intake for Case 3.1: using breast milk
- T.11 Rounded Calculation of Formula Mix to Meet Recommended Intake for Case 3.1: using breast milk
- T.12 Calculation of Formula Mix to Meet Recommended Intake for Case 3.1: using infant formula
- T.13 Recommended Nutrient Intake for Older Infants with MSUD
- T.14 Calculation of Current Nutrient Intake for Case 4.1
- T.15 Introduction of Solids for Case 4.1
- T.16 Sample Menu with Suggested Feeding Schedule for Case 4.1: infant with MSUD starting solids
- T.17 Recommended Nutrient Intake for the School-aged Child with MSUD
- T.18 Sample Menu for Case 5.1: school age child with MSUD
- T.19 Nutrition Goals During Acute Illness
- T.20 Monitoring During Acute Illness
- T.21 Recommended Nutrient Intake for Pregnant Woman with MSUD
- T.22 Recommended Nutrient Intakes for an Adult Woman with Classical MSUD (Non-pregnant)
- T.23 24-Hour Dietary Intake of an Adult Woman with Classical MSUD (non-pregnant)
- T.24 Calculation of Current Nutrient Intake for AC Prior to Pregnancy
- T.25 24-Hour Intake Modified for Increased Intact Protein
- T.26 Calculation of Current Nutrient Intake for AC at 30 Weeks Gestation
- References
- Contributors
- Appendix A: Recommendation Rating Definitions
- Appendix B: Terms
- Disclaimer
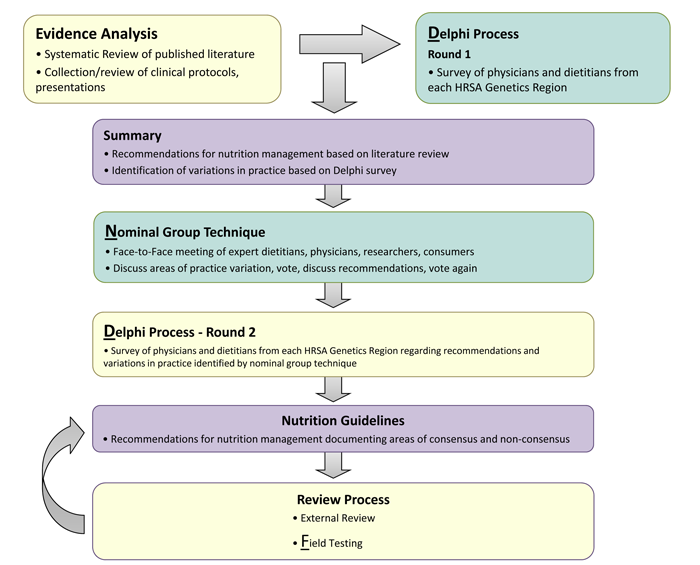
The Nutrition Guideline for MSUD is an evidence- and consensus-based management guideline created through a rigorous, transparent and systematic development process. The process was adapted from the Academy of Nutrition and Dietetics with the addition of specific techniques to draw on the expertise from clinical practice to fill in gaps where research is lacking. The process is published in the Journal of Evaluation in Clinical Practice and is available at http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2753.2011.01807.x/pdf. The process is illustrated in Figure 1, below:
Figure 1: Nutrition Guideline Development Process
Eight MSUD workgroup members independently identified over 40 practice questions where uncertainty and/or variation in practice existed. These were categorized into topics by the workgroup chair and resubmitted to members for prioritization. Five topics were identified for evidence analysis and guideline development:
- Nutrition management during illness and at the time of diagnosis
- BCAA levels
- Thiamin challenge/supplementation
- Nutrition management during pregnancy and the postpartum period
- Nutrition management in conjunction with liver transplantation
Research questions for each topic were formulated in the PICO (population, intervention, comparison, and outcomes) format, and a separate systematic review and evidence analysis was done for each question.
Because of the known scarcity of published scientific literature in nutrition management of IMDs, the search process included both published scientific studies and gray (practice) literature.
Scientific Literature: Search terms were specific to each question, but inclusion and exclusion criteria were the same for all questions. Eligibility was limited to human studies published in English from 1985 to summer 2011, with nutrition data included. For research related to thiamin, papers published as early as 1971 were included. There were no study design, age or setting restrictions. PubMed was the primary database used. Searches were conducted by a librarian at Emory University working in close collaboration with the project principle investigators, workgroup chair and project coordinator. The titles and abstracts of identified articles were scanned for relevance and matched with inclusion/exclusion criteria by the workgroup member responsible for the question. Excluded articles were noted and qualifying articles were gathered for review and abstracting. Reference lists within the identified articles were examined for additional resources. These were added if they contributed pertinent information.
Gray Literature: Gray literature refers to reports of clinical practice and research that cannot be accessed through standard search systems and includes abstracts and presentations from scientific and practice-based meetings, clinical protocols and guidelines, unpublished research, communication among experts (including listserves), professional newsletters, and chapters. The search for gray literature involved request to individuals (e.g., practitioners and researchers) and organizations for materials related to nutrition and MSUD. Identified resources were screened and prioritized for inclusion based on relevance, substantive information not available in scientific literature, and currency.
Each scientific article was critically reviewed by a trained analyst using a Quality Criteria Checklist, and the study design and methodology, findings, and author’s conclusions were abstracted to Evidence Abstract Worksheets. Quality criteria addressed: selection and retention of subjects, groups comparable, intervention clearly described and followed, other intervening variables tracked, outcomes defined, measures valid, and appropriate statistical analysis. Based on number of criteria met, each article was assigned a quality rating of positive, neutral or negative.
Gray/practice resources were reviewed by workgroup members using a specially developed quality criteria checklist for gray literature that included: clear purpose, relevance to intended users, systematic development process, clear clinical recommendations, applicable to practice, and free of conflict of interest. They abstracted clinical practices and outcome information onto worksheets.
Key information from all eligible evidence sources (scientific and gray literature) for each question was summarized on an evidence table, and an evidence summary and conclusion statement was drafted by a workgroup member and reviewed and edited by the workgroup chair and the Core Team.
Consensus-based input: many issues of concern to nutrition management were not addressed or were inconclusive from scientific and gray literature. For these issues, expert input from nutrition and medical clinicians and researchers was sought using a Delphi survey, nominal group process meeting and a second-round Delphi survey. By systematically employing these techniques, the level of agreement with specific practice statement was quantified.
Input of the target population (patient and family). A parent and leader of the MSUD Family Support Group participated in the nominal group process meeting. Further input will be solicited at the field testing phase.
The final conclusion statement for each question represented a synthesis of evidence from scientific publications, gray literature, and Delphi and nominal group consensus techniques.
Specific recommendations for nutrition management in each of the five topic areas were derived by the MSUD workgroup, in consultation with the Core Team, utilizing the evidence summaries, conclusion statements and the results of the consensus-based input. Each recommendation was rated with respect to strength (strong, fair, weak, consensus, insufficient evidence) and need for clinical action (imperative or conditional). See Appendix A: Recommendation Rating Definitions.
These practice recommendations along with background and other information to support their implementation are contained in the MSUD Nutrition Management Guideline document. The final document was reviewed, using AGREE II criteria, by an external panel of metabolic dietitians, physicians and an expert in guideline development methodology who were not involved in the evidence analysis or guidelines development phases. The guidelines are now available for dissemination and field-testing. The MSUD Nutrition Management Guideline can be accessed through the SERC and GMDI websites. An expanded version with the supporting evidence and consensus documentation is available to GMDI members.
Production of guidelines is achieved with a secure, web-based application written in PHP, MySQL and hosted by Apache HTTP running on a Linux server. Guidelines for an unlimited number of IMD can be supported with the application. For each IMD, forms exist for literature management, Delphi and Nominal survey management, and final guideline development. Published literature data is initially obtained via XML through the NCBI E-Utilities API. User-entered data is archived as changes are made, and content is locked through internal publishing prior to final guideline development. References for literature and tables are managed natively. Users are kept apprised of guideline development with automated email notifications. Built-in discussion forums are utilized for online group dialogue. Application security is maintained through use of SSL, user accounts and user-level access controls for each form. Backup is performed nightly. The complete MSUD Nutrition Management Guideline can be accessed through both the SERC and GMDI websites.
As a result of the evidence analysis and consensus processes, important areas for research were identified. Further, the practice recommendations outlined should lead to greater standardization of care and enable outcomes studies within and across centers. When warranted by developments in MSUD research and clinical practice, this guideline will be updated.


